




| Home | Features | Club Nights | Underwater Pics | Feedback | Non-Celebrity Diver | Events | 8 August 2025 |
| Blog | Archive | Medical FAQs | Competitions | Travel Offers | The Crew | Contact Us | MDC | LDC |

|

|
 
 |
  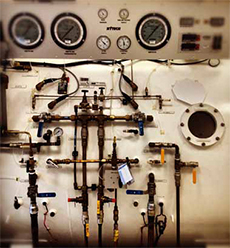 ISSUE 17 ARCHIVE - AT THE CHAMBERJoss WoolfI have had over twenty years of problem-free diving and clocked up a couple of thousand dives. Over the last nine years I’ve become a dedicated underwater photographer and member of The British Society of Underwater Photographers.They say that one of the first symptoms of decompression sickness is denial. We’d had a lovely week’s diving off the Isle of Man looking for those elusive basking sharks and enjoying our time with plenty of playful seals. I’d even skipped diving the day before the end of the trip, to spend it touring around this unusual British outpost. So when, on the morning of our departure, sitting on the ferry back to Heysham, I noticed that my right leg was numb, I instantly concluded it must be another sciatica attack; I’d had quite a bad one several years earlier which had left me with a slightly numb thigh. Back home, I went to work the next day, and to my great surprise, almost fell off a ladder! I should tell you, at this point, that as a curtain-maker I have been quite used to climbing up ladders for at least the last thirty years. I found kneeling difficult too, over the next few days; a sort of rather uncomfortable, spongy feeling. The numbness got worse and the leg got stiffer and I was obviously limping by the middle of the following week; enough to make me wonder... Could this possibly be a bend? Finally, on a Friday evening ten days after the first symptoms, I came home from a difficult day’s work, also up a ladder, and looked it up on the internet. Perhaps not surprisingly, numbness was quite high up on the list. First reaction, call the nearest hyperbaric chamber. Living in north London, I was lucky enough to have one on my doorstep, the London Diving Chamber in St John’s Wood, at St John and St Elizabeths Hospital. They said even if it wasn’t a bend, I was to go in straight away. What I hadn’t fully appreciated was that these chambers don’t have people manning them all the time, sitting around idly, waiting for the next bent diver to casually turn up off the street; but they have teams of people who are on call who can be there within twenty minutes, twenty-four hours a day. I got there at 6.30 on a Friday evening. We were due to go on holiday the next morning. After apologising for ruining all their Friday evenings, I was told that I would be surprised just how many people do leave it till a Friday night to make the call. After a thorough examination, it was determined that it was indeed a bend and not sciatica and I was faced with almost six hours in the chamber, using Royal Navy 62 tables. Three people were needed to look after me; one inside the chamber, in case of an oxygen seizure and two outside, in case of a problem with the accompanying nurse inside the chamber. “Have you eaten?” I was asked. I said I’d bought a sandwich in anticipation. “Oh, forget that, we have Sushi, or Thai, or Pizza! We’ll bring the takeaway menus into the chamber during the evening. We need to look after you!” Sure enough, after the initial 20 minute phases, with 5-minute mask-free breaks over, there was a small window of 15 minutes in which to eat our supper before being brought back to the surface from 18m. I’d chosen a modest portion of sushi but was told, hey c’mon, have more than that, you’re not paying! So I did. It’s quite boring having an oxygen mask tied over your face with an elastic band and it makes conversation difficult, so you definitely need reading material. I was finally released at 1.30 the next morning. The people looking after me couldn’t have been kinder. BUT, they wanted me back on Monday and I was going in just a few hours on our annual family holiday with fifteen members, to Dorset. At 9.00am, a few hours later, I took the liberty of calling the dive chamber in Poole, which wasn’t too far from where we would be staying. After he finally got used to the idea, Jim Booth agreed that I could go there for the rest of my treatment, starting Monday morning, but this was extremely irregular. It was only when I visited the Poole chamber that I learned that leaving it so long after the first symptoms could be extremely detrimental to the final outcome. I was extremely lucky. The sooner you can get treatment after the symptoms, the better the prognosis. You never know who you are going to meet inside a hyperbaric chamber. The people who agree to go on call are very often commercial divers, home for a break, or have professions related to diving in some way, or are nurses. All hyperbaric treatment for divers in the UK is NHS funded. Many of the chambers also offer other medical treatment, for example, to cancer patients, or diabetes sufferers with open ulcers/sores as the oxygen helps them to heal so much more quickly. But a lot of this very positive treatment has been withdrawn by the NHS, in some areas, due to cut-backs. (Visit Oxygen Healing to find out what conditions hyperbaric oxygen therapy can treat). On my first two days in Poole, I dry-dived with Tony, a commercial diver who frequently works on oil-rigs. He described working in Holland in seas of minus 27 and even after recompression on the surface for an hour following a saturation dive, he would come out of the chamber with 6” long icicles hanging off his dry suit. Next was a guy called Richard, who explained that his suntan had been acquired whilst skippering the film-crew’s boat for the Olympics on the Serpentine. He had covered the swimming marathon and the triathlon. It had been amongst some of the most difficult work of his life, going at only 2 knots an hour, to keep up with the swimmers and yet not create a wake. My last two days, I was escorted by young Steve who, amongst many other jobs, had skippered a boat from which giant wind turbines are installed in the sea in Denmark. At the end of my week, although I had significant improvement in the movement in my leg, I was a long way from being signed off. I was told I had suffered a spinal bend as it had affected the nervous system resulting in a loss of sensation and power, and I would need to come back in two months to be reassessed AND be tested for a PFO (patent foramen ovale). The PFO test, carried out in Bristol by Dr. Mark Turner, proved negative. The advice he gave was ideally to give up diving altogether since there had been no obvious cause for the bend. It could return at any time and the body’s ability to repair itself would now be compromised. Now that’s the thing; when diving is such an important part of your life, how can you make that decision? If I absolutely had to continue diving, he recommended the following: Lose a bit of weight, (more “mature” divers are more susceptible to a bend), get fitter and include some aerobic exercise, avoid dehydration, use nitrox on air tables, ensure that all your diving buddies are aware of the situation, take longer surface intervals between dives, ensure there is always oxygen available and establish where the nearest dive chamber is. |